Skull Base & Pituitary Tumor Program
3900 Pacific Coast Hwy, Newport Beach, CA 92663
(949) 764-4624
- About
- Conditions Treated
- About Skull Base Surgery
- Treatments
- Meet the Team
Ranked top-50 nationally for Neurology & Neurosurgery, offering minimally invasive care for complex tumors. Our multidisciplinary team uses advanced technology and precision techniques to ensure safe, effective treatment and the best possible outcomes.
Center of Excellence for Pituitary Surgery
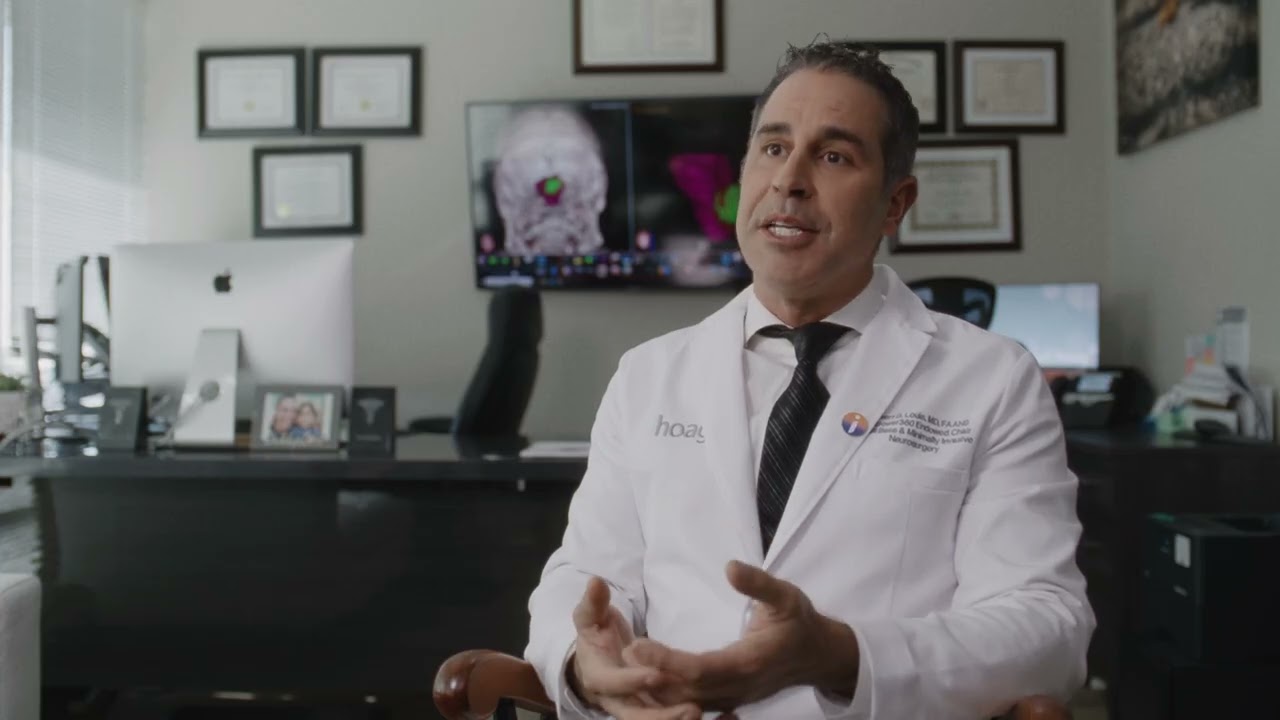
At Hoag’s Skull Base and Pituitary Tumor Program, patients receive world-class care from a team of highly specialized experts who redefine what’s possible in neurosurgery. Our fellowship-trained neurosurgeons, otolaryngologists, neurologists, neuro-ophthalmologists, neuroradiologists, and endocrinologists collaborate to deliver the safest, most effective treatment for even the most complex tumors. With decades of collective experience, our team has helped advance minimally invasive surgical techniques, prioritizing precision, safety, and patient recovery. Most procedures are performed through tiny incisions—or even through the natural passageways of the body, such as the nostrils—reducing pain, scarring, and recovery time. At Hoag, patients can trust that they are in the hands of pioneers who combine compassion, innovation, and advanced technology to achieve the best possible outcomes and quality of life.

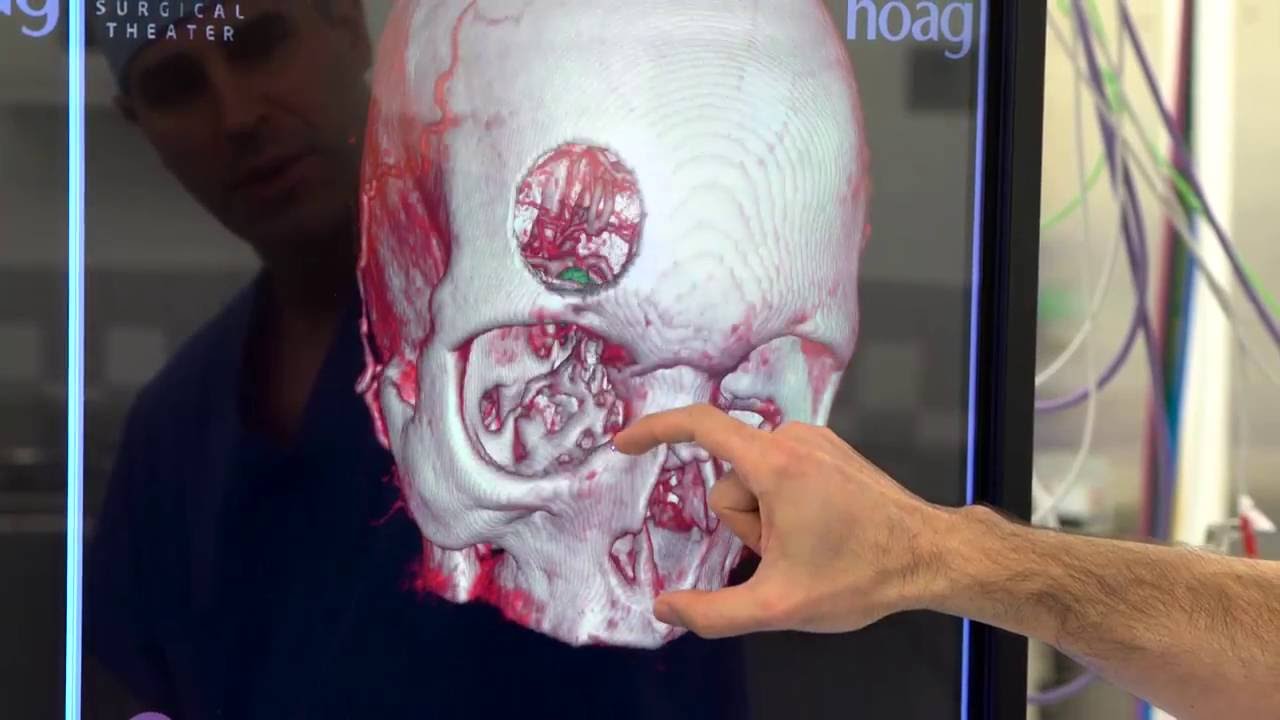
Precision in Motion: How Virtual & Augmented Reality Are Transforming Brain Surgery

Where Compassion Meets Innovation: A New Era of Patient Comfort
Healing starts with humanity. From our Styled for Surgery program to allowing patients to wear their own clothes, Hoag’s Skull Base and Pituitary Program blends world-class neurosurgery with a hospitality-inspired experience that helps you feel like yourself again. At Hoag, we understand that healing after brain tumor surgery isn’t just physical —it’s emotional, too. That’s why we’re offering a complimentary haircut service for anyone undergoing brain surgery. You’ll meet with Loni Kohlmyer, our licensed stylist, who will create a thoughtful hairstyle to gently conceal your incision, helping you move forward with comfort, confidence, and dignity. The day before surgery, Dr. Goldschmidt will mark the incision site. Then you’ll sit down with Loni to plan a look that feels right for you, showing as much or as little as you choose. Because healing should be personal, and you deserve to feel like you.